Fungal Infections
Fungal infections – the clinical problem
The occurrence of invasive fungal infections has risen in recent years, and is compounded by the difficulty of early and accurate diagnosis and appropriate use of antifungal therapy. The majority of serious fungal infections occur in hospitalized patients and those with compromised immune systems. Outbreaks of multi-drug resistant (MDR) fungal infections are therefore commonplace in the healthcare environment across the world.
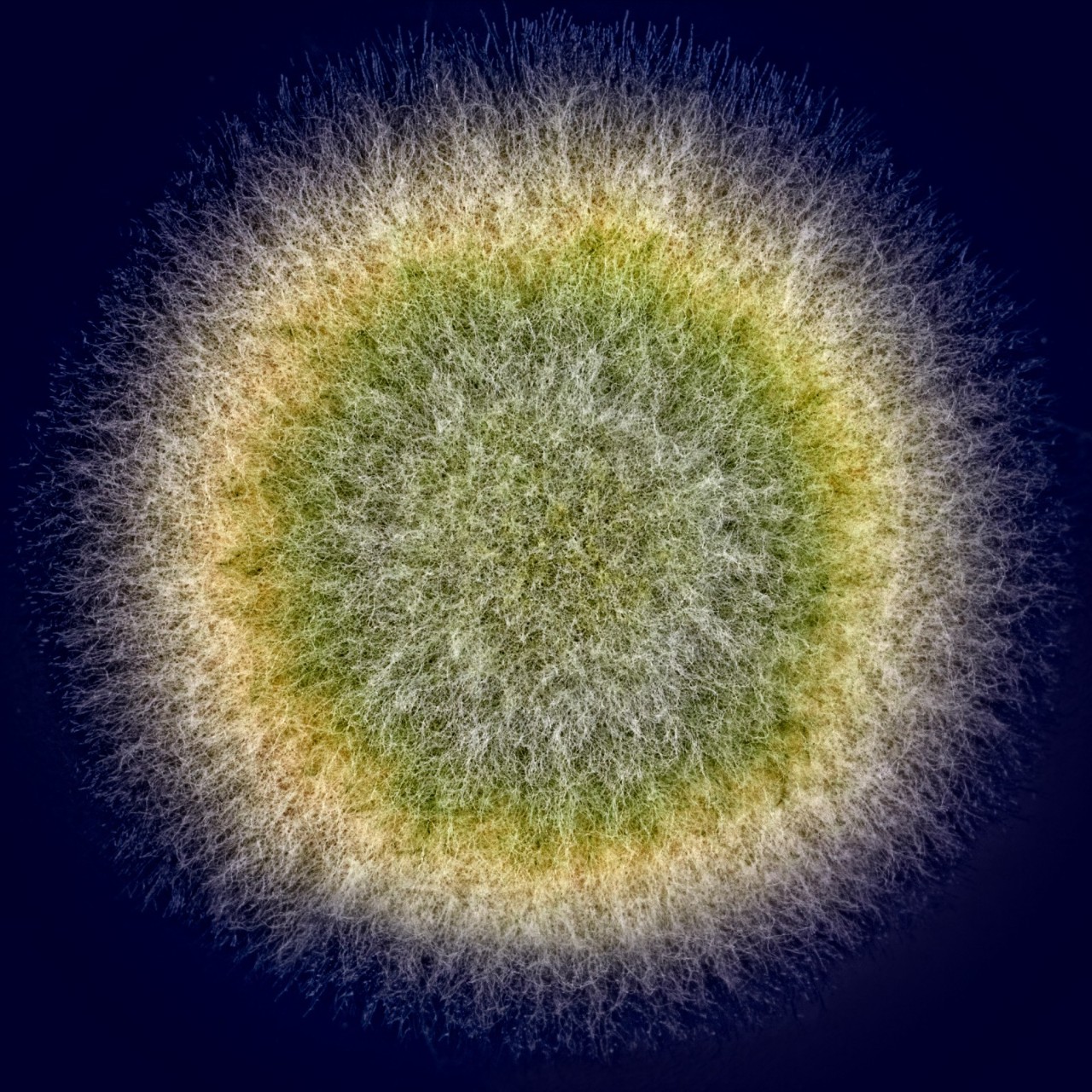
The identification of molds and multicellular fungi to the species level continues to be one of the most challenging aspects of microbiology, and hinders the timely delivery of life-saving treatment. However, recent advances in diagnostic tools are changing the outcome of fungal infections worldwide.
Rapid, culture-free detection
Traditional diagnostic methods for fungal infection include direct microscopic examination of clinical samples, histopathology, culture and serology. More recently, analytical tools such as mass spectrometry (MS) and molecular diagnostics have gained popularity in clinical laboratories.
If the sample has already been cultured, Matrix-Assisted Laser Desorption/Ionization Time-Of-Flight (MALDI-TOF) MS, such as the MALDI Biotyper®, provides reliable, accurate identification of fungi down to the species level.
For rapid, culture-free diagnostics, polymerase chain reaction (PCR) is an increasingly popular molecular technique.
Identification and susceptibility testing
PCR tools, such as Bruker’s Fungiplex® IVD assay solutions, allow clinicians to provide an unprecedented time-to-result in fungal infection cases. These real-time PCR assays ensure rapid, targeted results with high sensitivity and specificity, without relying on a lengthy culture process.
Due to the previous lack of specific identification methods, many fungal infections have been treated with broad-spectrum antimicrobial drugs, leading to MDR in some fungal species. Starting from a cultured sample, antimicrobial susceptibility testing (AST) can be run to establish whether the fungi in question, such as yeast or Cryptococci, are resistant to treatment.